While traditional bariatric surgery treats diabetes in obese patients, some procedures, such as Ileal Interposition, specifically treat diabetes even in patients who are not otherwise overweight.
Laparoscopic Ileal Interposition with SG is a promising procedure for the control of type 2 diabetes mellitus, hypertension, weight loss, and associated metabolic disorders.
Historical note on the Interposition of the ileum:
Insertion of the ileum is a new operation pioneered in Brazil for the treatment of type II diabetes. It was first introduced by Brazilian surgeon Aureo De Paula in 1999.
Surgical aspects of Ileum Interposition:
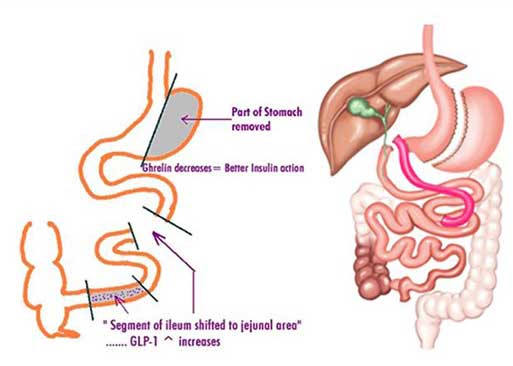
This surgery involves reducing the size of the stomach by a sleeve gastrectomy, in addition, the distal or final segment of the small intestine (ileum) is brought forward and connected to the initial or flexible small intestine (duodenum). Each surgical step in the Ileum Interposition procedure is designed to achieve a hormonal target.
Position of the patient in the operating room:

The position of the patient in this case is different, since this operation involves an operation in the lower abdomen. Thus, the patient is in the supine position after general anesthesia.
Iliac Interposition:
The procedure begins by creating a 170 cm segment of the ileum (the last section of the small intestine) and inserting it into the jejunum (middle section of the small intestine). There are three anastomoses or joints that can be made with staplers or sutures.
Hormonal mechanism of Ileum Interposition:
There are certain hormones that increase insulin sensitivity such as GLP-1 and certain insulin resistance hormones such as ghrelin, GIP, glucagon that are normally secreted in our gastrointestinal tract.
The goal of Ileal Interposition is to increase the production of insulin sensitivity hormones and leave out resistance hormones.
Resolution of diabetes and other comorbidities after Ileal Interposition:
Diabetes control after surgery is good, with patients demonstrating a reduction in the need for diabetes medications by more than 80%. Hypertension improves in more than (90%) patients. In the postoperative period, there is a significant decrease in microalbuminuria.
Recent studies have confirmed that IS with FH is effective even in non-obese diabetic patients with a BMI of 23–34 kg/m2 to improve their glycemic and metabolic disturbances. The key benefits of these studies are the safety and efficacy of surgery in the treatment of T2DM patients with lower BMI and metabolic improvement beyond glycemic control.
They showed a sustained improvement in glycemia with preservation of beta-cell function (pancreatic function) and a positive effect on the cardiovascular system.
Benefits of choosing AstraMedicaGroup
Only top qualified doctors
JCI certificated hospitals
Free COVID-19 Test before departure
4 nights in a 5-star hotel in Istanbul
Costs for laboratory, medication and equipment
Pre/post-operative tests
Free Istanbul tours
Latest technologies
Excelent travel assistance
All-round VIP transfer
Credit / Debit cards accepted
No prepayment
Personal assistants speak in English
24/7 customer service
